
Recent research has revealed a hidden but alarming consequence of hurricanes in the United States: an increase in death rates that can persist for up to 15 years after a storm has passed. While the immediate devastation caused by hurricanes is well-documented, a study published in Nature on October 2 uncovers the broader health impacts that remain uncounted.
As Hurricane Helene made landfall on September 26, 2024, it left a devastating path of destruction across Florida, Georgia, the Carolinas, and Tennessee, raising questions about the long-term health effects that may follow.
Helene, a Category 4 storm with sustained winds of 140 mph, tore through Florida’s Big Bend region before flooding communities across the Southeast. Thus far, the storm has claimed over 170 lives and displaced thousands, leaving communities reeling. But as the initial death toll from Helene is assessed, research suggests that the actual health impacts of the storm are far from over.
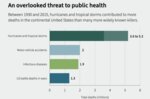
Official statistics traditionally record deaths caused by hurricanes during the event, often from trauma or drowning. However, the new study, led by Solomon Hsiang of Stanford University and Rachel Young of the University of California, Berkeley, estimates that a typical U.S. tropical cyclone indirectly causes 7,000 to 11,000 excess deaths. Since 1930, tropical storms may have contributed to 3.6 to 5.2 million deaths—far surpassing the death toll from motor vehicle accidents, infectious diseases, or wars in the same period. Officially, storm deaths total only about 10,000.
Based on data from 501 tropical cyclones between 1930 and 2015, these estimates build on prior research showing that storms slow economic growth for 15 years. A 2018 study found Hurricane Maria caused nearly 5,000 deaths in Puerto Rico, far exceeding the official count.
“In the months and years after a hurricane, people are dying earlier than they would have if the storm hadn’t hit their community,” Hsiang explained. These indirect deaths are linked to factors such as displacement, weakened social networks, economic hardship, and disrupted healthcare access. As recovery efforts in the aftermath of Hurricane Helene begin, it is crucial to consider these long-term health impacts.
These are infants born years after the cyclone, so they didn’t experience it directly,” Young explained, pointing to long-term economic and maternal health challenges that persist even years after the disaster.
Hurricane Helene’s unprecedented intensity can largely be attributed to climate change. The storm delivered catastrophic damage to the southeastern U.S., with North Carolina experiencing some of the worst flooding in its history. In Asheville, families were isolated by landslides and rising waters, with tragic outcomes. One family lost three members after their home’s roof collapsed under floodwaters, highlighting the deadly consequences of extreme weather exacerbated by climate change.
Helene’s record rainfall in North Carolina—over two feet in some areas—submerged entire towns. Experts estimate that the state will face billions in recovery costs, with the economic and health toll likely to linger for years. Similar storms have shown that recovery is only the beginning; the long-term health effects may include increased mortality rates among vulnerable populations.
Black Americans are three times more likely to die after a hurricane than white Americans, representative of the systemic inequalities in disaster response and recovery. Where marginalized groups are more likely to experience inadequate resources, slower recovery, and poorer health outcomes.
As seen with Hurricane Helene, vulnerable populations, including low-income communities and people of color, are often the hardest hit by extreme weather events' immediate and long-term consequences. In North Carolina, where recovery efforts are ongoing, these communities may face years of health and economic challenges due to the storm’s lasting impacts.
Hurricanes like Helene are becoming more frequent and severe due to climate change. Warmer ocean waters fuel these storms, leading to stronger winds and increased rainfall, making future hurricanes more destructive. Helene’s rapid intensification and massive storm surges, which affected coastal and inland areas alike, are harbingers of what’s to come in a warming world.
In response to these growing threats, experts emphasize the need for greater disaster preparedness and long-term recovery planning.
Research from Hsiang and Young’s team suggests that the health consequences of such storms often go unnoticed until years later when displaced families and financially strained communities struggle to cope with the lasting effects.
In addition to economic recovery, there is a need for healthcare systems and policymakers to anticipate and address the health burdens that follow disasters like Helene. “Some solutions might be as simple as ensuring that post-recovery plans include provisions for long-term healthcare needs,” Young explained. By focusing on the longer-term impacts of hurricanes, communities can better prepare for future storms and mitigate their hidden costs.